09. tbl. 108. árg. 2022
Management of patients with left main stem stenosis in Iceland 2010-2020: PCI or CABG
Meðferð höfuðstofnsþrenginga á Íslandi: Víkkun, hjáveituaðgerð eða lyfjameðferð?
Heiðrún Ósk Reynisdóttir1
Margrét Kristín Kristjánsdóttir1
Brynjólfur Árni Mogensen2
Karl Andersen1,2
Tómas Guðbjartsson1,3
Martin Ingi Sigurðsson1,4
Ingibjörg J. Guðmundsdóttir1,2
1Faculty of Medicine, University of Iceland, Departments of 2Cardiology, 3Cardiothoracic surgery, 4Anesthesiology & Critical Care, Landspitali - The National University Hospital of Iceland.
Correspondence: Ingibjörg J. Guðmundsdóttir, ig@landspitali.is
Key words: coronary artery disease, left main stem stenosis, PCI, CABG.
Introduction: Coronary artery bypass surgery (CABG) has been standard treatment for patients with left main coronary artery disease (LMCAD) but percutaneous coronary intervention (PCI) can be a good alternative. Our aim was to evaluate revascularization of LMCAD-patients in Iceland and treatment changes in recent years. We also assessed the impact of patient background factors on treatment choice and long-term survival.
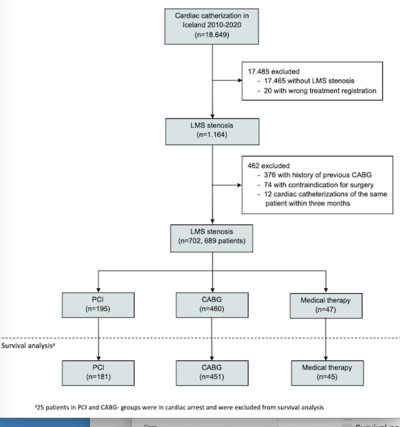
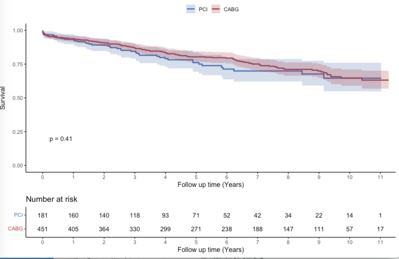
Methods: This retrospective, population-based registry-study analyzed data from the SCAAR-SWEDEHEART database. Patients with significant LMCAD on coronary angiography in Iceland 2010-2020, without previous history of CABG or contraindication for surgery were enrolled. The Kaplan-Meier method was used to study long-term survival and COX-regression analysis to adjust for predictor variables.
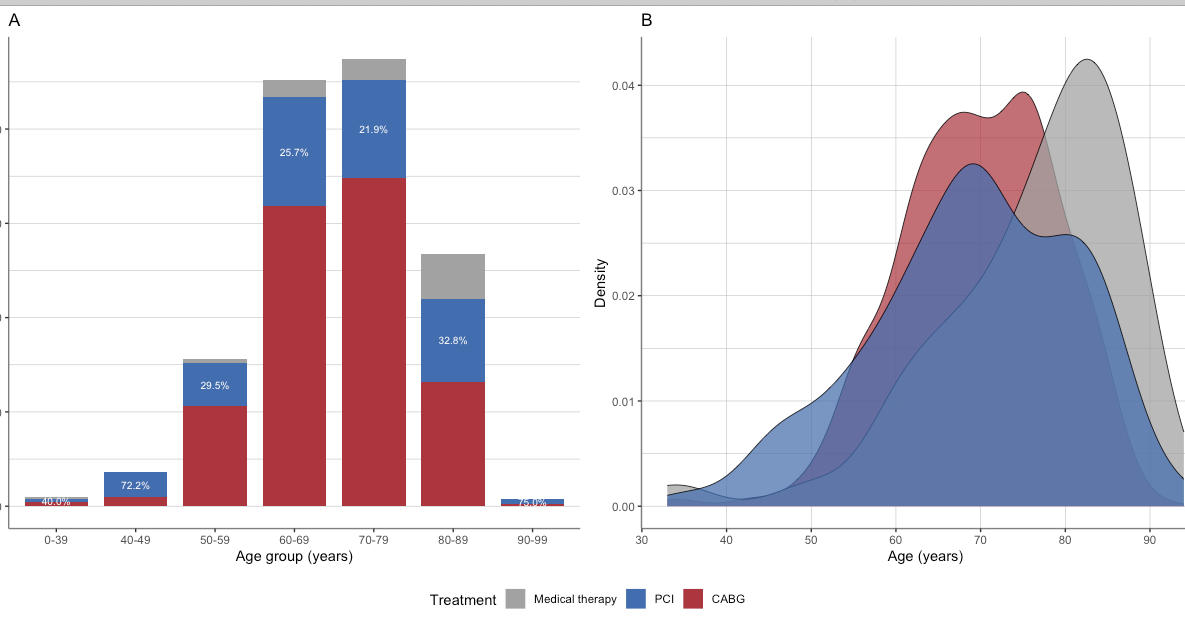
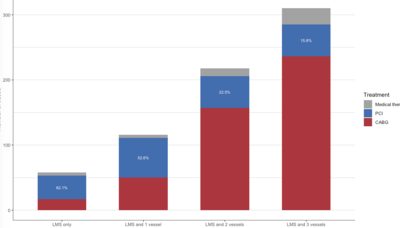
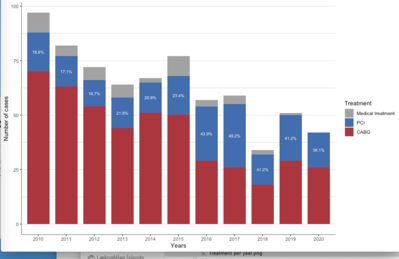
Findings: Of 702 LMCAD patients, 195 were treated with PCI, 460 with CABG and 47 with medical therapy. The widest age-range was in the PCI group and the mean age was highest in the medical therapy group. Patients with LMCAD and concomitant three vessel disease or heart valve disese were mostly treated with CABG (76.1% and 84.4%). The majority of patients with LMCAD only were treated with PCI, as well as patients presenting with STEMI or in cardiogenic shock (67.1% and 70.0%). The proportion of patients treated with PCI increased from 19.8% in 2010-2015 to 42.7% in 2016-2020. There was no significant difference in survival between the PCI and CABG-groups (p=0.41).
Conclusions: In patients with LMCAD the main factors determining treatment choice are age, anatomical complexity and acuteness. There has been a significant increase in LMCAD patients treated with PCI.
|
PCI (195) |
CABG (460) |
Medical therapy (47) |
p-value | |
| Age | 69.2 ± 12.0 | 69.7 ± 9.2 | 76.0 ± 11.3 | <0.001 |
| Female | 48 (24.6) | 86 (18.7) | 13 (27.7) | 0.118 |
| Body mass index [kg/m2] | 27.8 ± 4.4 | 27.9 ± 4.5 | 27.1 ± 3.6 | 0.565 |
| Diabetes | 33 (17.1) | 89 (19.5) | 8 (17.4) | 0.756 |
| Insulin | 14 (43.8) | 24 (27.3) | 4 (50.0) | 0.133 |
| Smoking | 39 (21.4) | 77 (17.0) | 5 (10.9) | 0.471 |
| Renal insufficiency | 53 (31.5) | 105 (24.1) | 22 (50.0) | 0.001 |
| Previous PCI | 45 (23.1) | 66 (14.3) | 11 (23.4) | 0.014 |
| Treated hypertension | 119 (63.0) | 299 (65.9) | 37 (84.1) | 0.027 |
| Cholesterol lowering drugs | 113 (59.5) | 302 (67.1) | 27 (58.7) | 0.128 |
| Previous myocardial infarction | 30 (16.6) | 72 (16.4) | 13 (28.3) | 0.125 |
| Cardiogenic shock | 21 (12.1) | 9 (2.5) | 0 (0.0) | <0.001 |
| Stable angina | 62 (31.8) | 161 (35.0) | 13 (27.7) | <0.001 |
| NSTEMI/unstable angina | 77 (39.5) | 228 (49.6) | 23 (48.9) | <0.001 |
| STEMI | 47 (24.1) | 20 (4.3) | 3 (6.4) | <0.001 |
| Heart valve disease | 2 (1.0) | 27 (5.9) | 3 (6.4) | <0.001 |