12. tbl. 99.árg. 2013
Epidemiology of needlesticks at Landspítali University Hospital during the years 1986-2011- A descriptive study
Faraldsfræði stunguóhappa á Landspítalanum á árunum 1986-2011. Lýsandi rannsókn
Introduction: Needlesticks, bodyfluid exposure and bites (incident) put healthcare workers (HCWs) at risk of hepatitis B, C and HIV particularly if patients are infected (high risk incident). The risk of infection is greatest from bore-hollow needles. The aim of the study was to describe the epidemiology of reported incidents and evaluate underreporting by HCWs at Landspítali University Hospital (LUH).
Methods: A retrospective descriptive study of reported incidents during 1986-2011. The ratio of incidents was calculated according to the HCWs age and profession and distribution by source and wards. The ratio of high risk incidents and vaccination status against HBV at time of incident was determined as well as underreporting during 01.01.2005-31.12.2011.
Results: At least 4089 incidents occured during the study period but 3587 were reported and blood samples taken from 2578 patients. Approximately a third of the incidents were associated with non-compliance with standard precaution and 54,7% of needlesticks were associated with bore-hollow needles. Few reports came from physicians and medical students (17,9%). During the study period 50,3% HCWs were vaccinated against HBV at time of incident. High risk incidents were 94 (2.6%), mostly related to hepatitis C (64,9%). Two HCWs became infected with HCV. During 2005-2011 underreporting was estimated to be 28,0%.
Conclusion: Improved education of standard precaution when handling needles and sharps at LUH may reduce the number of incidents. Introduction of safety-needles and safety-devices may greatly reduce needlesticks as a large number of incidents were associated with hollow needles. Improved HBV vaccination among HCWs and reporting incidents should be encouraged.
Key words: Sharps and needlestick injuries, blood and bodyfluid exposure, health care worker, Bloodborne pathogens, HBV vaccination coverage, occupational health.
Correspondence: Ásdís Elfarsdóttir Jelle, asdiself@landspitali.is
Jelle AE1, Hafsteinsdottir EJG1, Gudlaugsson O2, Kristjansson M2
1Department of quality and infection control, 2Department of internal medicine at Landspítali University Hospital.
Tables and figures:
Table 1. Overview, numbers of reported injuries, proportion of high risk injuries and proportion of health care workers vaccinated against HBV at time of injury during1986-2011.
| Year | Number of reported injuries | Proportion of high risk injuries | Proportion of health care workers vaccinated against HBV at time of injury | ||
| 1986 | 9 | 0 | 0,0 | ||
| 1987 | 7 | 0 | 0,0 | ||
| 1988 | 91 | 4,4 | 2,2 | ||
| 1989 | 126 | 0,8 | 5,6 | ||
| 1990 | 114 | 0,9 | 29,8 | ||
| 1991 | 75 | 0,0 | 29,3 | ||
| 1992 | 133 | 2,3 | 39,8 | ||
| 1993 | 139 | 0,0 | 35,3 | ||
| 1994 | 132 | 3,8 | 36,6 | ||
| 1995 | 94 | 0,0 | 37,2 | ||
| 1996 | 137 | 2,2 | 39,4 | ||
| 1997 | 153 | 3,3 | 22,9 | ||
| 1998 | 140 | 2,9 | 37,9 | ||
| 1999 | 143 | 4,2 | 51,0 | ||
| 2000 | 158 | 4,4 | 48,1 | ||
| 2001 | 154 | 0,6 | 42,2 | ||
| 2002 | 145 | 2,8 | 46,9 | ||
| 2003 | 145 | 1,4 | 46,2 | ||
| 2004 | 204 | 2,0 | 58,3 | ||
| 2005 | 210 | 5,2 | 52,9 | ||
| 2006 | 166 | 4,2 | 73,5 | ||
| 2007 | 173 | 0,6 | 71,7 | ||
| 2008 | 165 | 1,8 | 81,8 | ||
| 2009 | 196 | 3,6 | 78,6 | ||
| 2010 | 166 | 2,4 | 76,5 | ||
| 2011 | 212 | 5,2 | 81,1 |
Table II. Incidence of reported injuries at Landspitali University Hospital.
| Year | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 |
| Incidence/100.000 patients-day | 52,3 | 79,6 | 81,4 | 64,8 | 71,0 | 71,1 | 88,6 | 81,3 | 100,8 |
| Incidence /100 occupaid beds | 19,1 | 29,1 | 29,7 | 23,7 | 25,9 | 26,0 | 32,4 | 29,4 | 36,8 |
| Incidence /100 full-time equivalents | Missing | Missing | 4,9* | 5,7 | 5,6 | 5,3 | 6,2 | 4,7 | 7,5 |
* from 01.05.2005
Table III. Number of individuals diagnosted with HBV, HCV eða HIV in Iceland per year, per 100.000 inhabitands. Based on data from the homepage of the Directorate of Health, www.landlaeknir.is
| Year | HBV per 100.000 | HCV per 100.000 | HIV per 100.000 |
| 1997 | 8 | 20 | 3 |
| 1998 | 5 | 24 | 3 |
| 1999 | 16 | 30 | 4 |
| 2000 | 17 | 31 | 4 |
| 2001 | 21 | 27 | 3 |
| 2002 | 14 | 24 | 2 |
| 2003 | 8 | 13 | 3 |
| 2004 | 13 | 21 | 2 |
| 2005 | 11 | 15 | 3 |
| 2006 | 5 | 18 | 4 |
| 2007 | 15 | 31 | 4 |
| 2008 | 19 | 29 | 3 |
| 2009 | 7 | 33 | 4 |
| 2010 | 9 | 19 | 8 |
| 2011 | 9 | 23 | 7 |
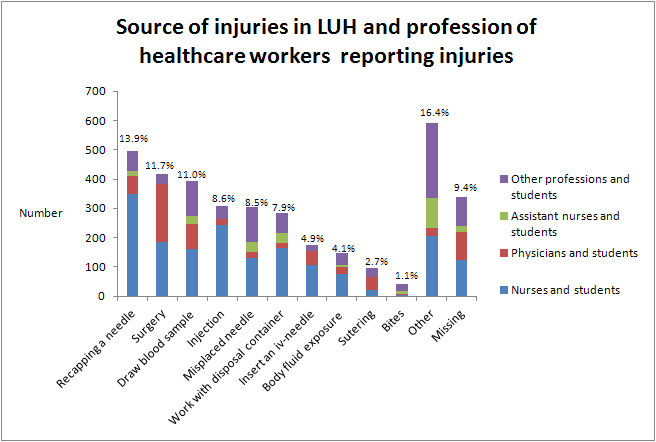
Figure 1: Proportion of reported injuries by wards during 1986-2011.
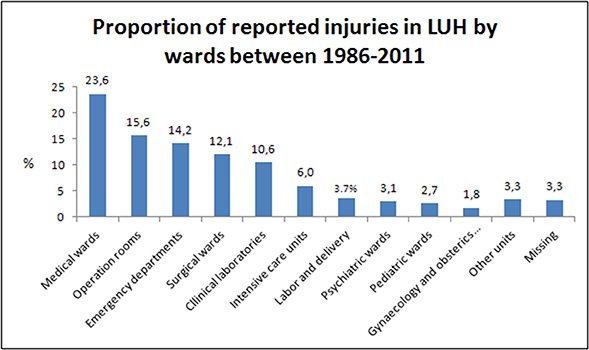
Figure 2: Source of injuries by healt care workers professions during 1986-2011.