04. tbl. 111. árg. 2025
Patients diagnosed with C. difficile infections (CDI) at Landspítali University Hospital from 2017-2022
Rannsókn. Clostridioides difficile iðrasýkingar á Landspítala 2017-2022
Clostridioides difficile iðrasýkingar á Landspítala 2017-2022
Arnar Þór Sigtryggsson1Kristján Orri Helgason2Agnar Bjarnason1,3Magnús Gottfreðsson1,3
1Faculty of Medicine, School of Health Sciences, University of Iceland; 2Department of Clinical Microbiology, Landspitali University Hospital; 3Department of Infectious Diseases, Landspitali University Hospital
Corresponding author: Magnús Gottfreðsson, magnusgo@landspitali.is
Abstract
Objective: To investigate the epidemiology, severity, treatment, and prognosis of patients with C. difficile infections (CDI) diagnosed at Landspítali University Hospital from 2017-2022.
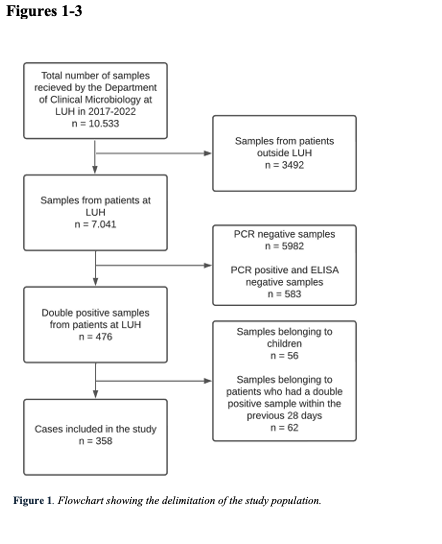
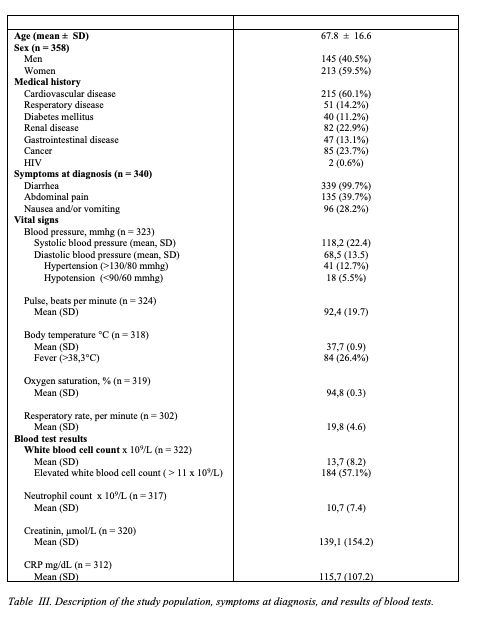
Materials and Methods: The study population consisted of adult patients at Landspítali with double-positive (PCR + ELISA) diagnostic tests. If the same patient had two or more positive samples within a 28-day period, they were considered to reflect the same infection, and the latter samples were excluded.
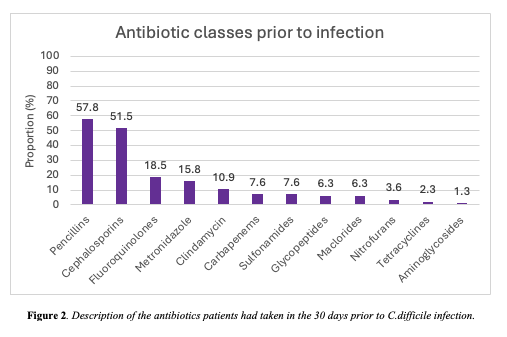
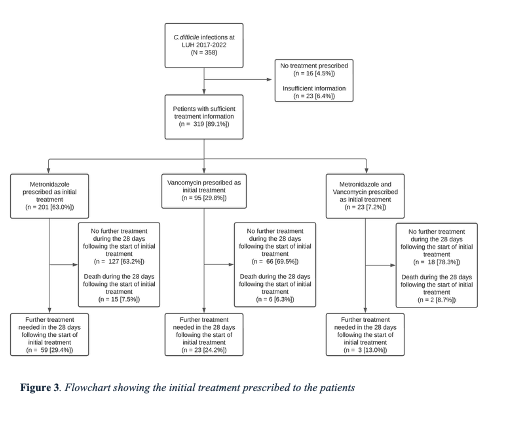
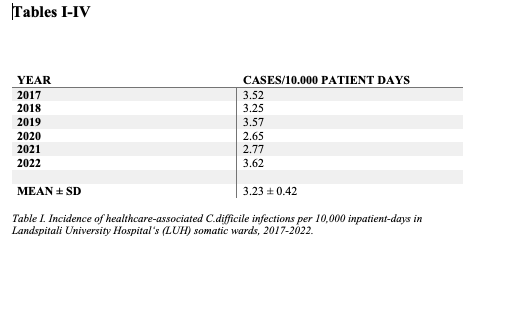
Results: Overall, 358 CDI were identified in 301 patients. The majority of cases were diagnosed in women (59.5%). The incidence of healthcare-associated CDI was 3.23 infections/10.000 in-hospital days (range 2.65 – 3.26). Incidence of community-associated CDI was 0.57 infections/10.000 inhabitants of the Reykjavik metropolitan area. Incidence was positively correlated with increasing age and remained similar throughout the study period. The recurrence rate during the study period was 15.3% with a mean follow-up period of 1.6 person-years. At least 85.5% of patients had taken antibiotics within a month before diagnosis, most commonly from the penicillin class (57.8%), followed by cephalosporins (51.5%). More than half (54.7%) of patients had taken proton pump inhibitors preceding diagnosis. Metronidazole was the most common initial treatment (63.0%). Of these, 29.4% of cases required further treatment within 28 days of treatment start. Fecal microbiota transplantation was performed in 13 cases. The all-cause 30-day mortality rate was 7.3%.
Conclusions: The incidence of CDI at Landspítali has remained stable and comparable to what has been reported in Europe during the same period. Most patients had one or more risk factors present. Most received antibiotics as treatment, most commonly metronidazole. The results of this study indicate that incidence and clinical presentation of CDI in Iceland are stable, whilst novel treatment options look promising.